Across the U.S., the stakes for medical malpractice are rising. Recent cases like New York's $80M award to a man whose family alleges he received substandard prenatal care make it clear that healthcare organizations need to be proactive to reduce harmful events instead of reacting after it's too late. Providing inadequate care in 2022 comes with a staggering price tag.

Early resolution programs seek to communicate, resolve or settle adverse incidents before they escalate to expensive litigation. Beyond improving care, effective early resolution programs can improve a healthcare organization's culture to best catch incidents and find system flaws before they hurt patients and providers. Candace Eden, a Joint Commission consultant who helps hospitals pass quality inspections, calls this a 'culture of safety'. Here are three tips for building a culture of safety in your health organization.
Easy Areas for Improvement
From her experience finding risks in hospitals, Candace shares several common areas for improvement that organizations of any size can investigate. For example, CMS considers many hospital-acquired infections as 'never-events' and will not reimburse for cases. Therefore, risk leaders must prioritize proper wound care and patient turning. One type of hospital-acquired injury, decubitus ulcers, accounted for 60,000 claims and can set back a 300-bed hospital up to $10 million in unreimbursed costs.
Eden highlights another surprising area of risk: improper equipment usage. The Joint Commission has seen a significant increase in improper equipment usage due to complacency. For example, a physician leader incorrectly explains how to use a device, and faculty continue to recreate the error because they trust the leader's expertise. Reviewing equipment instructions with staff is a surefire and inexpensive way to reduce this risk.
Equipment misuse can have severe consequences. For example, the CDC identified at least 49 outbreaks of infectious materials due to improper vial use, which resulted in over 150,000 patients needing to be notified.
Building Healthcare Transparency
Creating a transparent, accountable care culture, while not as straightforward a measure as reducing equipment misuse, can help healthcare organizations further realize a zero-harm events goal. Transparency works on a patient-provider level. Providers can make corrections before issues arise if patients feel comfortable speaking up about subpar care.
Healthcare organizations can implement a series of measures to give space for concerned patients to speak up. A straightforward way to add transparency to treatment plans is using patient teach-back. Often, healthcare workers trust that patients understand a diagnosis or treatment's implications. By having the patient reiterate the information in their own words, staff can guarantee that they processed it. Teach-back benefits are two-fold. First, it helps the patients advocate for themselves and navigate their treatment. Secondly, it ensures that patients can explain the information to their families or other providers, preventing misunderstandings and readmissions.
Likewise, proper transparency extends to the organization's C-suite. Upper-level hospital staff can avoid the risk of providers hiding mistakes by keeping an open line of communication with caregivers. Candace Eden recently discussed an example of organization-wide transparency with Medplace.

We created a video series called "It Could Happen to You." For example, an episode had a nurse that told their story of leaving a sponge in a patient after surgery and what we could do to make that not happen again. We got great feedback when we sent those videos out to all the staff. You've got to be open and talk to your patients talking to your consumers, your families, and your team. If they're comfortable, they'll speak up.
Communication Between Organizations
Transparency can continue beyond a health system. Industry efforts like state-level risk management organizations give leaders forums to share information. Traditionally, healthcare leaders viewed speaking openly about malpractice and areas of risk as taboo, but according to Eden, an open dialogue is a way forward for improving patient safety.

Attorneys feared that if we disclosed errors, patients wouldn't come to us, but it's completely the opposite. I worked to have the leaders from all of the facilities that [The Joint Commission] worked with to disclose errors. We shared them, and it was revolutionary for these leaders. They had never heard what each individual hospital had done and what they did to make it from happening again. But that prevents harm everywhere.
"It Could Happen to You," and collaborative efforts like it show that speaking frankly about hospital risk creates a culture of safety and reduces risk. Eden spearheaded the joint effort between FSHRMPS (Florida State Healthcare Risk Management and Patient Safety), ACHA, the Florida Nurse Association, and more to provide education about avoiding risk and resolving cases early. This communication helps spread lessons learned in risk management to other organizations, so they do not need to learn firsthand through their own adverse events.
Culture of Safety and Early Resolution
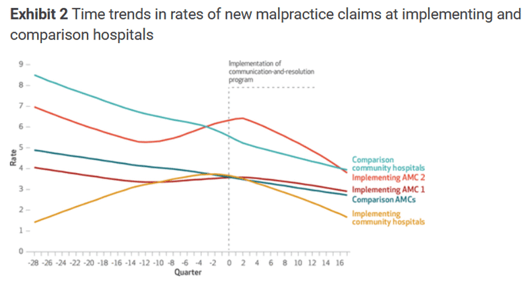
Taking steps to communicate and resolve cases before they escalate to litigation comes with tangible results, and building a culture of safety plays an instrumental role in early resolution. A study published in Health Affairs found trends pointing to lower case volumes and severity following the implementation of a CRP (Communication Resolution Program).
To see how external peer reviews can help your healthcare organization resolve cases and improve safety, schedule a Medplace demo today.



